Hey there! Have you ever wondered how our mood and mental health are connected to the tiny powerhouses within our cells called mitochondria? Well, buckle up because we’re about to dive into a fascinating topic: “Mitochondria and Depression: New Insights into the Development of Mood Disorders.”
Now, mitochondria may not be the first thing that comes to mind when we think of depression, but recent research has shed light on their role in our emotional well-being. These little energy factories are responsible for generating the fuel our cells need to function properly. But it turns out, their impact goes beyond just powering our bodies. They also play a crucial role in regulating our brain chemistry and influencing our mental state.
In this article, we’ll explore the exciting new findings that link mitochondria to depression. We’ll uncover the intricate relationship between these tiny organelles and our mood, and how dysfunction within them can contribute to the development of mood disorders. So, get ready to embark on a journey through the microscopic world of mitochondria and discover the hidden connections between our cells and our mental health. Let’s get started!
Recent research suggests a potential link between mitochondria, the powerhouses of our cells, and the onset of depression. Scientists have discovered that dysfunctional mitochondria may contribute to the development of mood disorders. This groundbreaking discovery opens up new possibilities for understanding and treating depression. By targeting mitochondrial function, researchers hope to uncover novel therapeutic approaches that could provide relief for millions of individuals suffering from mood disorders. Stay tuned for further updates as this research continues to unfold.
Mitochondria and Depression: New Insights into the Development of Mood Disorders
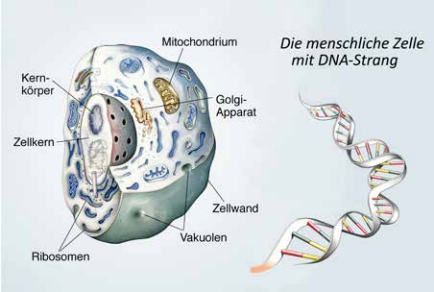
Mitochondria are often referred to as the powerhouse of the cell, responsible for producing energy in the form of adenosine triphosphate (ATP). However, recent research has revealed that these tiny organelles may play a much larger role in our overall well-being, particularly when it comes to mental health. In this article, we will explore the connection between mitochondria and depression, uncovering new insights into the development of mood disorders.
The Role of Mitochondria in Mental Health
Mitochondria are not only involved in energy production but also play a crucial role in various cellular processes, including calcium signaling, oxidative stress regulation, and apoptosis. Emerging evidence suggests that mitochondrial dysfunction may contribute to the development of psychiatric disorders, including depression. Dysfunction in mitochondria can lead to a decrease in ATP production and an increase in reactive oxygen species (ROS) generation, resulting in oxidative stress and cellular damage.
Studies have shown that individuals with major depressive disorder (MDD) often exhibit alterations in mitochondrial function. These alterations may include decreased mitochondrial respiration, impaired mitochondrial DNA (mtDNA) integrity, and abnormalities in mitochondrial morphology. Additionally, mitochondrial dysfunction may disrupt neurotransmitter signaling pathways, such as the serotonin and dopamine systems, which are implicated in mood regulation.
Impact of Mitochondrial Dysfunction on Neuroplasticity
Neuroplasticity refers to the brain’s ability to adapt and reorganize itself in response to environmental and internal changes. It plays a crucial role in learning, memory, and emotional regulation. Mitochondria are essential for maintaining proper neuroplasticity, as they provide the necessary energy for synaptic transmission and plasticity-related processes.
Research suggests that mitochondrial dysfunction can impair neuroplasticity, contributing to the development and progression of depression. Reduced ATP production and increased oxidative stress can lead to synaptic dysfunction and neuronal damage, disrupting the delicate balance of neurotransmitters involved in mood regulation. These alterations may result in structural and functional changes in brain regions implicated in depression, such as the prefrontal cortex and hippocampus.
Mitochondrial Dysfunction and Inflammation in Depression
In addition to its role in energy production, mitochondria also play a crucial role in immune system regulation. Mitochondrial dysfunction can trigger an inflammatory response, characterized by the release of pro-inflammatory cytokines and activation of immune cells. This chronic low-grade inflammation has been implicated in the pathogenesis of various disorders, including depression.
Depression is often associated with increased levels of inflammatory markers in the blood and cerebrospinal fluid. These markers include cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha). Studies have shown that mitochondrial dysfunction can stimulate the production of inflammatory cytokines, perpetuating a cycle of inflammation and oxidative stress in the brain.
The Gut-Brain Axis and Mitochondrial Function
The gut-brain axis refers to the bidirectional communication between the gastrointestinal tract and the central nervous system. Growing evidence suggests that disturbances in gut microbiota composition, known as dysbiosis, can influence brain function and contribute to the development of psychiatric disorders, including depression.
Interestingly, mitochondrial dysfunction has been linked to dysbiosis and altered gut microbiota composition. The interaction between the gut microbiota and mitochondria plays a crucial role in maintaining mitochondrial function and overall metabolic homeostasis. Disruptions in this interaction can lead to impaired energy production, increased oxidative stress, and inflammation, all of which are associated with depression.
In conclusion, emerging research suggests that mitochondria play a significant role in the development of mood disorders, including depression. Mitochondrial dysfunction can disrupt energy production, impair neuroplasticity, trigger inflammation, and contribute to the dysregulation of neurotransmitter systems. Understanding the link between mitochondria and depression may pave the way for novel therapeutic strategies targeting mitochondrial function and restoring cellular homeostasis in individuals with mood disorders. Further research is needed to elucidate the underlying mechanisms and develop targeted interventions for mitochondrial dysfunction in depression.
Mitochondria and Depression: New Insights into the Development of Mood Disorders
Recent studies have revealed the potential role of mitochondria in the development of depression and mood disorders.
- 1. Mitochondria are tiny structures found in cells that produce energy.
- 2. Dysfunction in mitochondria may contribute to the development of depression.
- 3. Mitochondrial dysfunction can disrupt the production of neurotransmitters, affecting mood regulation.
- 4. Research suggests that targeting mitochondrial function could be a potential treatment for depression.
- 5. Further studies are needed to fully understand the relationship between mitochondria and depression.
Häufig gestellte Fragen
What are mitochondria and how are they related to depression?
Mitochondria are small organelles found in our cells that are responsible for producing energy. They are often referred to as the powerhouses of the cell. Recent studies have shown a potential link between mitochondrial dysfunction and depression. When mitochondria are not functioning properly, they can lead to an imbalance in neurotransmitters and a decrease in energy production, which can contribute to the development of mood disorders such as depression.
Furthermore, mitochondrial dysfunction can also lead to oxidative stress and inflammation, which are believed to play a role in the pathophysiology of depression. Understanding the relationship between mitochondria and depression is crucial for developing new treatment strategies and improving our understanding of the underlying mechanisms of this complex disorder.
How do mitochondrial abnormalities contribute to the development of mood disorders?
Mitochondrial abnormalities have been observed in individuals with mood disorders such as depression. These abnormalities can result in a decrease in energy production and an increase in oxidative stress, both of which can have detrimental effects on neuronal function and overall mental health.
Studies have shown that individuals with depression have lower levels of mitochondrial DNA and reduced mitochondrial activity in certain brain regions. Additionally, mitochondrial dysfunction can impair the production of neurotransmitters such as serotonin and dopamine, which are crucial for regulating mood and emotions. By understanding the role of mitochondrial abnormalities in mood disorders, researchers can explore new avenues for targeted treatments.
What are the potential causes of mitochondrial dysfunction in depression?
There are several factors that can contribute to mitochondrial dysfunction in individuals with depression. One potential cause is genetic predisposition. Certain genetic variations can affect the structure and function of mitochondria, making individuals more susceptible to developing mood disorders.
Other factors that can contribute to mitochondrial dysfunction include chronic stress, inflammation, and exposure to toxins. These factors can disrupt mitochondrial function and lead to a decrease in energy production and an increase in oxidative stress. By identifying the underlying causes of mitochondrial dysfunction, researchers can develop more targeted interventions to prevent or treat mood disorders.
Can improving mitochondrial function help alleviate symptoms of depression?
Emerging research suggests that improving mitochondrial function may be a potential therapeutic target for individuals with depression. Strategies aimed at enhancing mitochondrial function, such as exercise, dietary interventions, and supplementation with certain nutrients, have shown promise in improving depressive symptoms.
Additionally, medications targeting mitochondrial dysfunction, such as mitochondrial enhancers and antioxidants, are being explored as potential adjunctive treatments for depression. By improving mitochondrial function, it is possible to restore energy production, reduce oxidative stress, and potentially alleviate symptoms of depression. However, further research is needed to fully understand the mechanisms and effectiveness of these interventions.
What does the future hold for the study of mitochondria and depression?
The study of mitochondria and its link to depression is still in its early stages, but it holds great potential for advancing our understanding and treatment of mood disorders. As researchers continue to unravel the complex relationship between mitochondrial dysfunction and depression, new therapeutic targets may emerge.
Future studies may focus on developing more specific interventions that target mitochondrial abnormalities, as well as identifying biomarkers that can help diagnose and predict treatment response in individuals with depression. By expanding our knowledge of mitochondria and its role in mental health, we may be able to develop more effective and personalized treatments for individuals with depression.
Was ist Depression wirklich? | SWR Wissen
Abschließende Zusammenfassung: Shedding Light on the Connection Between Mitochondria and Depression
After diving into the fascinating world of mitochondria and its potential role in the development of mood disorders like depression, it is clear that we have uncovered some intriguing insights. While the exact mechanisms are still being explored, emerging research suggests that dysfunction in mitochondria may contribute to the onset and severity of depressive symptoms. These findings open up new avenues for understanding and treating depression, offering hope to millions of individuals who may be affected by this pervasive condition.
The link between mitochondria and depression highlights the intricate interplay between physical and mental health. Mitochondria, often referred to as the “powerhouses” of our cells, play a crucial role in energy production and cellular function. When these tiny organelles malfunction, it can disrupt various cellular processes, potentially impacting brain function and mood regulation. This connection underscores the importance of a holistic approach to mental health, recognizing the complex web of factors that contribute to our emotional well-being.
Moving forward, further research is needed to unravel the precise mechanisms underlying the mitochondria-depression connection. Scientists are exploring potential therapeutic interventions that target mitochondrial function, aiming to restore balance and alleviate depressive symptoms. By shedding light on these new insights, we pave the way for innovative treatments that could revolutionize how we understand and manage depression. As we continue to unlock the mysteries of the mind and body, the potential for improved mental health outcomes becomes an exciting possibility.